close
Choose Your Site
Global
Social Media


Views: 0 Author: Site Editor Publish Time: 2025-07-14 Origin: Site











Flow sensors have become a cornerstone technology in modern medical equipment, particularly for devices that monitor and assist patient respiration. By accurately measuring the flow rate, volume, and pressure of gases—most commonly oxygen and air—flow sensors enable clinicians to monitor, control, and optimize breathing therapies. Their importance spans from critical care environments like intensive care units (ICUs) to ambulatory and home care settings, diagnostic laboratories, and emergency medical services.
The integration of precise flow sensing technology enhances the safety and effectiveness of respiratory support devices. It empowers healthcare providers to detect early signs of respiratory distress, adjust ventilator settings in real time, and deliver customized therapies tailored to individual patient needs. Additionally, flow sensors contribute significantly to accurate diagnosis and monitoring in pulmonary function tests.
Mechanical ventilators are lifesaving devices used primarily in ICUs to support patients unable to breathe adequately on their own due to illness, injury, or surgery. They assist by delivering controlled air or oxygen mixtures into the lungs and removing exhaled gases. At the heart of these devices lie sophisticated flow sensors that measure the inspiratory and expiratory airflow precisely.
These sensors enable continuous, real-time monitoring of several key respiratory parameters:
Tidal volume: The amount of air delivered or breathed in during a single breath.
Respiratory rate: Number of breaths per minute.
Minute ventilation: Total volume of air exchanged per minute.
Peak inspiratory pressure: Maximum pressure applied to the lungs during inhalation.
By providing accurate data on these variables, flow sensors allow ventilators to dynamically adjust ventilation modes and parameters to patient needs. For example, in volume-controlled ventilation, the sensor confirms the target tidal volume is delivered. In pressure-controlled modes, it helps prevent excessive pressure that can injure delicate lung tissue.
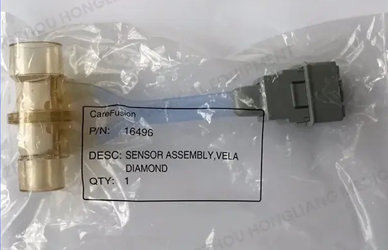
A leading example in this category is the Bird VELA Flow Sensor, which works in conjunction with an exhalation valve to maintain optimal ventilation. The flow sensor uses a combination of thermal mass flow and pressure-based technologies to provide precise measurements with minimal resistance, ensuring patient comfort and safety.
The accompanying exhalation valve regulates the release of exhaled gases, helping to maintain the desired airway pressure and prevent rebreathing of carbon dioxide. This integrated system supports ventilation for both adult and pediatric patients and is known for its robustness and reliability in critical care environments.
Beyond hospitals, ventilators are also employed in home care for patients with chronic respiratory conditions such as COPD, ALS, or spinal cord injuries. Portable home ventilators incorporate miniaturized, low-power flow sensors that extend battery life while maintaining measurement accuracy. These devices enable patients to maintain mobility and independence without compromising respiratory support.
Neonatal respiratory care is an especially demanding application for flow sensors. Premature infants and newborns have extremely sensitive and underdeveloped lungs, requiring highly gentle ventilation with extremely small tidal volumes—often less than 10 milliliters per breath.
The flow sensors used in neonatal ventilators must detect very low airflow rates with exceptional accuracy and low dead space to avoid increased respiratory workload. They also need to be biocompatible and often disposable to reduce infection risks.
The GE 1505-3272-000 Neonatal Flow Sensor is designed specifically to meet these needs. Using advanced thermal mass sensing technology, it accurately measures the delicate airflow patterns of neonates, enabling clinicians to closely monitor breathing and adjust support accordingly.
This sensor's compact size and minimal resistance allow it to be incorporated into tight neonatal circuits without adding stress on the infant’s respiratory system. Its disposable nature ensures hygiene, essential for reducing hospital-acquired infections in neonatal intensive care units (NICUs).
By providing precise respiratory data, neonatal flow sensors help prevent common complications such as bronchopulmonary dysplasia and ensure the infant receives adequate oxygenation and ventilation.
Anesthesia machines administer volatile anesthetics and other gases to maintain unconsciousness and pain control during surgeries. Flow sensors play a crucial role in regulating the flow rates and pressures of these gases, ensuring patient safety and effective anesthesia.
In operating rooms, flow sensors monitor both inhaled and exhaled gas volumes to help maintain the correct mixture of oxygen, anesthetics, and other gases. Real-time flow data allows anesthesiologists to adjust gas concentrations dynamically, avoiding underdosing, which can lead to patient awareness during surgery, or overdosing, which can depress vital functions.
Anesthesia flow sensors must endure the demanding environment of surgical suites. They require resistance to repeated sterilization and exposure to a variety of gases and humidity levels. Commonly, these sensors employ thermal or ultrasonic technologies for rapid response and high accuracy.
Their robust construction ensures long service life despite frequent handling. Additionally, they must be sensitive enough to detect subtle changes in flow and pressure during the complex phases of anesthesia delivery, including induction, maintenance, and emergence.
Emergency medical services (EMS) rely on ventilators equipped with flow sensors that perform accurately in harsh, unpredictable conditions. Ambulances, helicopters, and disaster response units often transport critically ill patients requiring ventilation.
Sensors in transport ventilators must be compact, lightweight, and shock-resistant, capable of maintaining accuracy despite vibrations, temperature fluctuations, and variable power availability. This portability ensures patients receive continuous, high-quality respiratory support during rapid transfers or field operations.
Accurate flow monitoring during transport is critical to prevent hypoxia and respiratory failure. The sensors enable paramedics to monitor ventilation parameters remotely and make adjustments on the fly.
Their reliability and durability can mean the difference between life and death in pre-hospital care and during inter-facility transfers, underscoring the vital importance of flow sensor technology in emergency medicine.
Pulmonary function testing is a cornerstone in diagnosing and managing chronic respiratory diseases. Spirometry, the most common PFT method, requires precise measurement of airflow during forced inhalation and exhalation maneuvers.
Flow sensors in spirometers capture detailed airflow patterns that allow calculation of lung volumes, airflow obstruction, and airway responsiveness. These data points help diagnose diseases such as asthma, chronic obstructive pulmonary disease (COPD), and restrictive lung disorders.
PFT flow sensors are typically ultrasonic or differential pressure sensors, selected for their fast response times and wide dynamic range. They are designed to handle rapid changes in airflow from gentle breaths to forceful exhalations, maintaining accuracy throughout.
Modern devices integrate digital outputs and software analytics, making flow sensors an essential component for delivering reliable, reproducible test results that guide clinical decision-making and monitor disease progression or treatment efficacy.
Flow sensors are indispensable in a broad spectrum of medical applications involving respiratory care. Their ability to provide accurate, real-time airflow data underpins the safe and effective operation of ventilators, neonatal devices, anesthesia machines, emergency transport ventilators, and pulmonary diagnostic equipment.
As technology advances, flow sensors continue to improve in sensitivity, durability, and integration capabilities, supporting better patient monitoring and therapy customization. For healthcare providers and medical device manufacturers, sourcing high-quality, compatible flow sensors is essential to ensuring optimal device performance and patient outcomes.
Hangzhou Hongliang Medical Equipment Co., Ltd. offers a wide range of premium flow sensors compatible with major brands such as GE Datex-Ohmeda, Dräger, and Bird. To explore our product catalog or receive expert consultation tailored to your specific medical device needs, visit www.hzhlmedical.com or contact our professional team today.
