close
Choose Your Site
Global
Social Media


Views: 0 Author: Site Editor Publish Time: 2025-11-08 Origin: Site











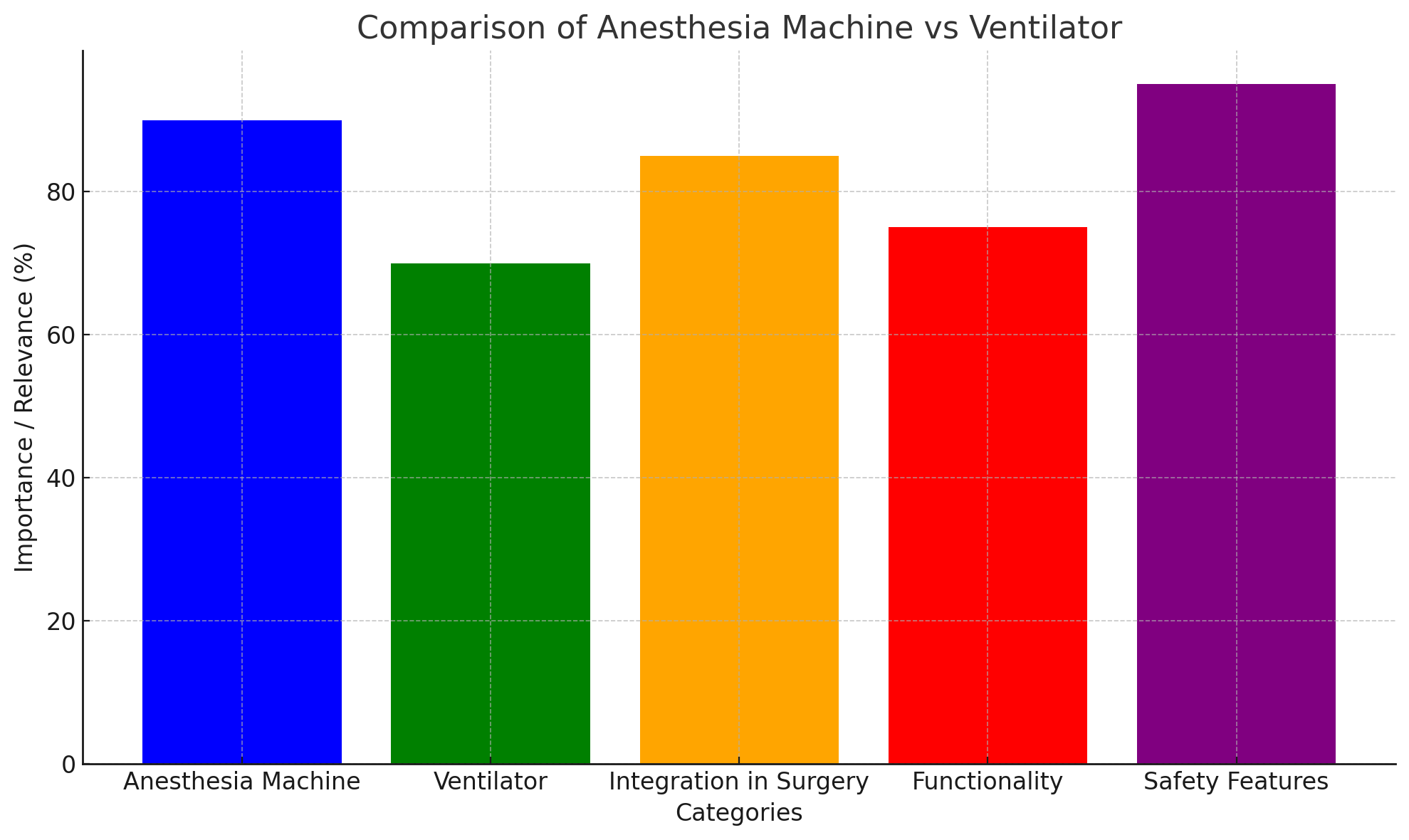
Anesthesia machines are vital in surgeries that require unconsciousness. But, do they function as ventilators? This question is crucial in understanding their role in patient care. While both devices manage breathing during surgery, they serve different purposes. In this article, we will explore the key differences between an Anesthesia Machine and a ventilator, and clarify their distinct yet complementary functions in healthcare settings.
An Anesthesia Machine is a complex piece of equipment used to deliver anesthetic agents and gases, including oxygen, to a patient during surgery. It ensures that the patient remains unconscious, pain-free, and ventilated throughout the procedure. The primary components of an anesthesia machine include:
● Gas delivery system: Delivers oxygen, nitrous oxide, and anesthetic gases.
● Vaporizer: Precisely mixes volatile anesthetics into the gases.
● Breathing circuit: Ensures the patient receives and exhales gases properly.
● Ventilator: A mechanical device that supports the patient's breathing when they are unable to breathe on their own.
● Safety systems: Monitors and manages gas flow, ensuring the patient’s safety at all times.
Yes, many modern Anesthesia Machines include a built-in ventilator. This ventilator helps maintain the patient’s oxygen levels by providing controlled breathing support during the surgery. While the anesthesia machine is responsible for delivering anesthesia and oxygen, the ventilator ensures the patient’s lungs are properly ventilated, especially when the patient is under general anesthesia and unable to breathe independently.
The ventilator may be manually controlled or fully automated, depending on the complexity of the anesthesia machine and the patient’s needs.
A ventilator is a medical device designed to assist or replace a patient’s breathing. It is commonly used in situations where a patient is unable to breathe on their own, such as during surgery, in intensive care units, or in emergency settings. Ventilators can be used for both short-term and long-term respiratory support, and they come in various types depending on the mechanism of action and the clinical setting.
Ventilators deliver air or a mixture of gases into the patient’s lungs, ensuring that they receive adequate oxygen and expel carbon dioxide, which is vital for maintaining stable blood gas levels.
While ventilators and Anesthesia Machines share some similarities, their functions differ. The primary role of a ventilator is to manage the patient’s breathing, while the anesthesia machine focuses on delivering anesthetic gases and oxygen to maintain unconsciousness and stable physiological function.
Key differences include:
● Ventilators can provide more comprehensive respiratory support by offering different modes of ventilation, such as volume-controlled and pressure-controlled ventilation.
● Anesthesia machines provide a specific setup designed for controlled anesthesia delivery and incorporate a ventilator to assist with breathing, especially in general anesthesia settings.
In an operating room, an anesthesia machine often doubles as a ventilator but with a narrower scope of function tailored to the needs of anesthesia and surgery.
Anesthesia machines are designed to support the patient’s ventilation needs during surgery. These machines integrate a ventilator that helps supply a controlled amount of air or oxygen when the patient cannot breathe on their own due to muscle paralysis caused by general anesthesia.
Modern anesthesia machines may offer various ventilation modes, including:
● Volume-controlled ventilation: Delivers a set volume of air to the patient.
● Pressure-controlled ventilation: Maintains a certain pressure throughout the respiratory cycle.
The ventilator integrated into the anesthesia machine ensures that the patient receives adequate ventilation throughout the procedure, as breathing ability is often compromised under anesthesia.
Anesthesia machines and ventilators can differ in their power sources. While some ventilators are purely mechanical and rely on manual control, anesthesia machines often incorporate both electrical and pneumatic components. This dual-source power enables the machine to deliver anesthetic gases and oxygen while ensuring patient safety during surgery.
Anesthesia machines typically use compressed gas or electrical power to drive the ventilation system. For example, a modern anesthesia machine may use a piston ventilator, which uses electricity to power the motor that drives gas flow, or a bellows-type ventilator, which relies on compressed gas to function.
Many anesthesia machines provide both manual and mechanical ventilation options. During the initial stages of anesthesia, the anesthesiologist may manually squeeze the bag connected to the anesthesia machine, providing intermittent positive pressure ventilation. However, as the surgery progresses, the mechanical ventilator takes over, providing more precise and continuous breathing support.
This flexibility allows anesthesiologists to tailor ventilation to the patient’s condition and the surgery’s needs. The mechanical ventilator is typically set to deliver air at a consistent rate, while the manual method allows for more flexible control when needed.
The Anesthesia Machine provides ventilation by integrating a ventilator system that ensures the patient receives a constant flow of oxygen and anesthesia gases. In addition to supporting the patient’s breathing, the machine is equipped with sensors to monitor oxygen levels, respiratory rate, and other vital signs, which are crucial during surgery.
The anesthesia machine can also adjust ventilation parameters based on the patient’s condition, providing volume-controlled or pressure-controlled ventilation, as needed. This ensures the patient’s oxygen and carbon dioxide levels remain balanced, preventing complications such as hypoxia or hypercapnia during surgery.
Most modern anesthesia machines integrate mechanical ventilators that are used in conjunction with the anesthetic delivery system. This integration ensures that while the anesthesia machine is delivering gases to the patient, the ventilator is maintaining the required levels of ventilation.
The combination of an anesthesia machine and a ventilator improves the safety and efficiency of the procedure, ensuring the patient is effectively sedated and ventilated throughout the surgery.
Anesthesia machines and ventilators evolved separately but gradually began to integrate in modern healthcare settings. Initially, ventilators were separate devices used primarily in intensive care and emergency medicine, while anesthesia machines were designed to deliver anesthetics during surgery.
However, over time, the need for more comprehensive patient care during surgery led to the integration of ventilators into anesthesia machines. Today, both devices are often used interchangeably, leading to confusion about whether an anesthesia machine is technically a ventilator.
In most surgical environments, the line between anesthesia machines and ventilators blurs because both are used to manage the patient’s breathing during surgery. While anesthesia machines provide ventilation as part of their functionality, they are not the same as the standalone ventilators used in intensive care units or emergency medicine.
Ensuring that patients can breathe properly during surgery is critical to their safety. Anesthesia machines, equipped with ventilators, are responsible for maintaining this vital function by delivering precise amounts of oxygen and anesthetic gases, depending on the patient’s needs.
The proper functioning of these systems is essential to avoid complications such as hypoxia, a condition in which oxygen levels in the blood drop dangerously low. Continuous monitoring and adjustments are made by anesthesiologists to ensure that ventilation is adequate throughout the procedure.
Anesthesia machines are equipped with a variety of safety mechanisms to monitor and ensure proper ventilation. These include alarms for low oxygen levels, disconnected circuits, or improper ventilation rates. In case of any irregularities, these alarms prompt immediate intervention to safeguard the patient’s health.
In summary, an Anesthesia Machine includes a ventilator but serves a broader role. It provides both anesthesia and ventilation support during surgery. The ventilator ensures effective breathing management under anesthesia. With advancements in technology, both anesthesia machines and ventilators continue to improve, enhancing patient safety and surgical outcomes. Hangzhou Hongliang Medical Equipment offers high-quality anesthesia machines that provide reliable ventilation support, ensuring optimal care during surgical procedures.
A: An anesthesia machine includes a ventilator but serves a broader purpose. It provides both anesthesia and ventilation support during surgery.
A: The anesthesia machine delivers oxygen and anesthetic gases while ensuring the patient's breathing is supported during surgery, often integrating a ventilator.
A: The ventilator in an anesthesia machine ensures that the patient continues to breathe effectively by providing mechanical ventilation during surgery.
A: No, an anesthesia machine is primarily used during surgery for anesthesia delivery and breathing support, unlike general ventilators used in intensive care.
A: Understanding the difference helps clarify their roles in patient care. An anesthesia machine combines both anesthetic delivery and ventilation, while a ventilator focuses solely on breathing support.
